Period pain, or dysmenorrhoea, is the crampy pelvic pain that occurs with your menstrual period. Just over 70% of young people experience some pain with their period. For some it is very mild but for others it can be very severe. Period pain is usually worse the first couple of days of bleeding or when the bleeding is at its heaviest.

Why do I get period pain?
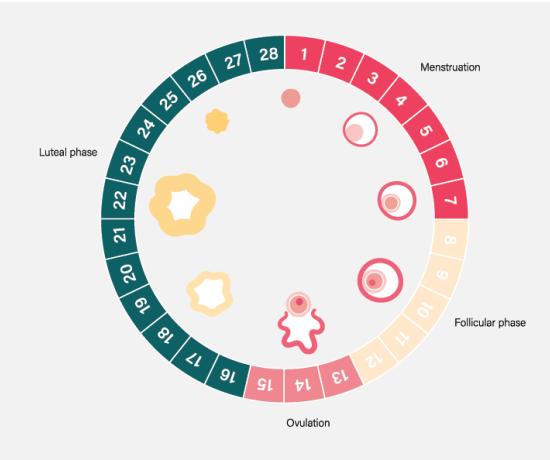
Periods occur when the lining of the inside of the uterus (womb) is shed in the absence of pregnancy. This usually happens once every calendar month although period frequency can range anywhere between 21-35 days. The number of bleeding days for a period varies greatly from one person to another but it usually takes 2-7 days (average 4 days) for the lining of the uterus to shed.
The reason you get cramps in the lower tummy with menstrual periods is due to inflammatory chemicals called prostaglandins. To help shed the lining of the uterus, our very clever bodies release prostaglandins that help the lining come away. Prostaglandins also help the uterus to cramp which helps push menstrual blood out of the uterus and into the vagina so it can leave the body. Some people release a lot of prostaglandins so will tend to have worse cramping pain. Others hardly have any cramps but still have a normal period and manage to expel (push out) the old lining from inside the uterus without any issues. Prostaglandins also act on other muscles and blood vessels in the body and can cause diarrhoea around your period, make you feel faint, or have headaches.
What happens during the menstrual cycle?
After a period, the inside lining of the uterus is quite thin. Different hormones stimulate the lining to thicken in time for ovulation (mid-cycle) so that if you fertilise an egg (get pregnant), the uterus is ready to grow a baby. If there is no fertilisation this month, the lining will gradually break down and then come away as a period.
Why do my periods hurt so much?
Usually your period hurts because you release a lot of prostaglandins, which are inflammatory chemicals. There are some other ideas about period pain that suggest that the uterus in some people doesn’t always cramp from top to bottom (to push blood out) and/or squeezes very tight around the cervix (opening of the womb/uterus) causing more pain and a slow release of blood. Some people experience blood clots with their periods which can vary in size. Menstrual blood that pools will tend to form clots and you may, for example, notice more clots in the morning when you first get up.

Period pain and endometriosis
For people with endometriosis, additional period pain can occur because the areas of endometriosis might also be flooded with prostaglandins causing additional inflammation and irritation at the time of a period. Some other signs that what you are experiencing may be more than typical period pain are:
- Period pain that starts well before you start bleeding (2 days or more)
- Pain is so severe that you may not be able to get out of bed or function normally (you need to stay home from school or work)
- Pain medications may not help manage the period pain
- You may still have severe pain even if you are taking an oral contraceptive pill or other hormonal medication (e.g. Implanon, Nuvaring, Mirena, Depo injections)
- Severe period pain may have started early in your adolescent years
- You may experience pain when passing a bowel motion (poo) or doing a wee
- You may experience painful sex
- You may be experiencing a delay falling pregnant
- Your mother, sister, grandmother or other family members may also have very painful periods
- You may experience severe pain during ovulation

Following research in over 2,000 Australian teenagers in Canberra, a screening tool called ‘PIPPA’ (Period ImPact and Pain Assessment) has been developed with five questions that you can answer to see if you have problematic periods. Your score out of five will guide you about what to do next. Whatever your PIPPA score is, if you have concerns about your periods and feel that you need to see your GP, then you should do so. You can find the PIPPA tool here and it also forms part of the EndoZone Health Report, which you can print out to take to your doctor.
Things you can do for period pain:
For ideas on how to manage period/pelvic pain you can visit EndoZone’s Self-Management section, or try some of the ideas below:
- Heat packs - Can help blood circulation in the pelvis and soothe cramping muscles
- Massage - Gently massage your tummy in a clockwise direction with a nice oil
- Stretches for pelvic pain - A visit to a pelvic physiotherapist can also help.
- Movement plans – There is some evidence to suggest that exercise can assist with reducing the intensity of pain. Try light exercise such as walking to improve pelvic circulation and release pain relieving chemicals in your body.
- Simple eating – the gut often doesn’t like rich and spicy foods before a period although you may crave sweet foods. Small, healthy, simple meals are best to help manage bloating and other possible symptoms like constipation or diarrhoea.
- Rest and sleep - Get plenty of rest and sleep
- Manage and reduce stress – get support if you need it, treat yourself gently, and perhaps try some of the relaxation exercises on EndoZone
- Medications to suppress your period - Consult your doctor about suitable medications to reduce period symptoms.
- Acupuncture - Some research suggests that acupuncture can have beneficial effects on pain severity in those with endometriosis.
View all self-management options

When should you see your doctor?
- If period pain does not allow you to go to work or school or interferes with other daily activities.
- If you experience severe period pain.
- If you experience pain during urination.
- If you experience pain with bowel movements or while doing a poo.
- If you experience pain in your lower abdomen without a period.
- If you feel emotionally or mentally overwhelmed due to period pain.
Please note, you may find it beneficial to work with a range of different healthcare professionals such as, GP, gynaecologist, psychologist, pelvic physiotherapist etc. to manage your pain better.
 Skip to main content
Skip to main content