Sex should not be painful but 61% of people with endometriosis report experiencing pain during sex (dyspareunia) and some can continue to experience pain after sex too. If sex has been painful for some time then you will likely have more than one type of pain as the body/brain tries to protect you, creating further symptoms. Many things can cause sex to be painful and it is important for you to understand what might be causing pain for you.
People of different ages can experience sexual pain and, regardless of age, finding a way to manage painful sex is important. There are a number of reasons why sex may be painful and it is important to remember painful sex is far more common than you think and you are not alone.

A healthy, pain-free sexual relationship, either with yourself and/or another person, can influence how you feel about yourself and your relationships with other people. Sexuality includes a variety of factors, including sexual feelings, interest, and activity, and varies considerably between people. Sexuality is not just physical; it has psychological, emotional and spiritual meaning as well. Your relationship with your body is an important component of your sexuality. How comfortable you are with your body – how it feels and responds and what brings pleasure – actually makes a big difference to your experience of sex.
Each person will generally have things that enhance or increase their sexual responses and other factors that have the opposite effect and decrease their desire or inhibit their sexual response. Pain during and after sexual activity can act as a desire inhibitor because it impacts your ability to enjoy sexual intimacy. Life is hectic and stressful and we don’t often give enough time for proper arousal and relaxed pleasurable sex. It can take a while to switch off from the day and try to focus on your body’s sensations and what you are feeling rather than your ‘To Do’ list. If you are tense, you may not feel the pleasurable sensations that you otherwise might feel. An orgasm can be a great release. But if your muscles are super tight, then they may spasm and lead to more pain. All of this influences your experience of sex and how you respond to sexual difficulties (e.g. whether you try to address them or whether you tend to avoid sex). If you have concerns about sex or are experiencing pain, consulting a GP, local sexual health service, pelvic health physio, psychologist or a Sex and Relationships Therapist may be useful.
Sex can hurt for lots of reasons – read on…
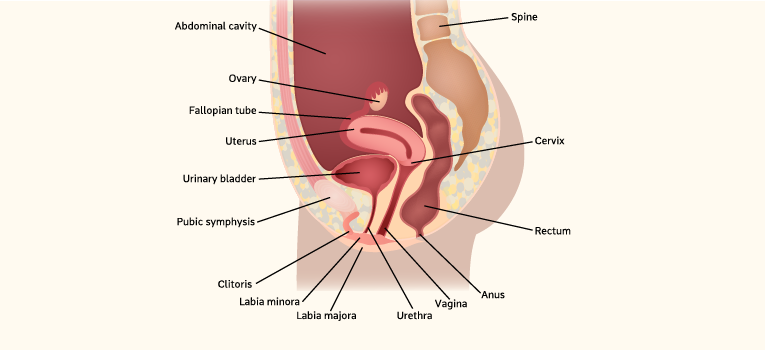
The pelvis is a busy place with lots of things happening. Not only does it house your reproductive organs, but also your bowel (digestion and poo) and your bladder (wee). In fact the bladder is in front of the vagina and the bowel behind it, right next to each other. Then there are all the muscles, ligaments, bones, nerves, blood vessels and the lymphatic system.
Not surprisingly, many things can contribute to sex being painful. Often people have more than one thing causing their pain and often they are not things we can see or touch. Memories of past experiences or worries about pain or our bodies can stop us from feeling relaxed and may contribute to feeling pain. Some people may have tried to manage their sexual pain by trying to ignore it or to ‘push past it’. Unfortunately, this can create a vicious cycle because it often results in increased muscle tension which leads to more pain.
The things that can cause pain and discomfort with sex and how to tell the difference
For the purpose of this article, we will concentrate on sex with penetration (sexual intercourse). To identify what might be contributing to the issue, we will start at the outside of the vagina and then work our way in. If you have been diagnosed with endometriosis, don’t assume that it is causing all of your pain. It is a good idea to book an appointment with your GP to discuss your symptoms so they can help you identify the cause(s) and refer you to other practitioners as needed (e.g. gynaecologist, pelvic health physio, psychologist, sex therapist). You may need to see a range of health professionals about your sexual pain, depending on the cause. Your specialist will ask questions so that they can work with you to understand your sexual pain experiences. This means that they will most likely ask you where the pain is located (e.g. vulva, deep inside the vagina), how the pain developed, and what it is currently like (e.g. burning, stabbing). It is important to tell your specialist about the impact that painful sex has had for you as an individual or in relationships.

Sometimes it can be difficult to find the right person that you feel comfortable talking to. Some doctors and health professionals may also struggle with these conversations. However, people who deal with sexual pain all the time will have no trouble discussing the detail, so you may like to find a health provider that specialises in sexual health. Some suggestions for managing different sexual pain have been provided below, but it is best to work with your health care team so you get the right management strategies for you. For additional information see the links at the end of this article.
| Pain Type | Feels or Looks Like | Talk to your GP About | What might help |
|---|---|---|---|
| 1 | Burning or stinging at entrance of vagina (beginning or during sexual intercourse) May get better or worse during intercourse Pain with touch | Lack of lubrication Vulvodynia |
|
| 2 | Walls of vagina are itchy (can make sex unpleasant) Changes in discharge (thick, white ‘cottage cheese’, grey, watery appearance, yeasty or ‘fishy’ smell) | Thrush/ Bacterial Vaginosis |
|
| 3 | Something stopping penetration Painful or tight feeling when something is inserted (penis, tampons, finger/s, sex toys) May not be able to have intercourse or starts off okay and then worsens | Muscles around or inside the vagina (pelvic floor muscles) are tight or contract which makes intercourse difficult/painful. Known as vaginismus or GPPPD (Genito Pelvic Penetration Pain Disorder) Ask GP/gynae about other things that might be stopping easy penetration, other than tight muscles. |
|
| 4 | A deeper pressure, dull achy pain, spasm (can become sharp or stabbing type pain during/after sex or with orgasm) | Deeper pelvic muscles too tight or ‘switched on’ instead of relaxed. Common for those that experience pain with sex – related to brain’s protective response to pain in the pelvis – it protects the body by tightening the muscles |
|
| 5 | Sharp pain with deep penetration (feels like being poked deep inside) May vary with sexual position Or may get more painful leading up to or during a period | May be related to endo pain If had this pain for a long time may develop brain’s protective response of tightening the muscles (see Pain Type 3 or 4) |
|
There are a range of other types and causes of pain with sex which need to be followed up with your GP, sexual health service or gynaecologist including sexually transmitted infections (STIs e.g. Herpes, Chlamydia), bladder or urinary tract Infections, any types of lesions, growths, infections, or cervical cell changes. It’s important to get regular testing for STIs and to undergo a pap smear to check for cervical changes. Always protect yourself from STIs by using a condom – it’s just not worth the risk.
Pain with sex – it’s complicated…
If you have had painful sex for a long time you will need to invest in your sexual self to understand your symptoms, causes and treatment options. It is also important to be honest with how you think about sex. We are all products of our environment, culture, family, religion and upbringing which can colour how we view sex – e.g. as something shameful, dirty and bad; a way to connect with others; something that just feels good; something fun and exciting; or something we only want to share with special people. We all have different views and attitudes to sex. One thing is clear, your body image and how you feel about yourself (including self respect) will be important to how you view sex.

Sex with other people raises questions around your consent and boundaries, and can be further complicated by the use of alcohol or drugs. Experiences such as sexual assault and rape can greatly affect our view and experience of sex and lead to protective physical responses that we may not even realise are happening. Seek out appropriate counselling through rape crisis services, hotlines, psychologists or sex therapists. You do not need to deal with this on your own.
If there are long term difficulties surrounding sex in a relationship, it commonly leads to relationship breakdown if couples don’t work as a team to overcome issues. It’s best to identify and face the issues so you can feel better about yourself, your relationship, and minimise the impact on your relationship (and move away from the guilt and shame often experienced). Seek counselling, psychology or sex therapy to assist with this.
Sex pain and fertility – for people with endo, trying to conceive generally means coming off any hormonal medication used to manage endo symptoms. You may be worried about sex pain while you are trying to fall pregnant. During this time, complementary therapies such as acupuncture and some herbs can help manage endo or period pain symptoms as well as increase your chances of falling pregnant. It is best to consult health practitioners who specialise in this area of fertility.
Libido is another related issue and usually multiple causes are involved including hormone levels, hormonal medication, other medications, overall health, body-image, self-image, the connection and relationship with your partner (especially communication), fears, stress, and previous sexual experiences. Engage your healthcare team to discuss your symptoms and concerns.
Additional resources:
- Endometriosis Australia: Pelvic Floor
- Jean Hailes: Relationships and Sex
- EndoActive: Sex, intimacy and endo
- Royal Women's Hospital: Fact Sheet
- International Pelvic Pain Society – Patient Handouts
- Book: Emily Nagoski 2021 Come as you are, Simon & Schuster Paperbacks, New York; (video)
 Skip to main content
Skip to main content